How it went wrong for the UK, and why you need to secure your PPE supply chain
Covid-19 has been a challenging time which has highlighted the importance of not just keyworkers, but healthcare supply chains too. Weaknesses and vulnerabilities in supply chains have been exposed, which is impacting the delivery of healthcare, as well as ordering PPE for healthcare.
This article looks at how the UK is handling the distribution of PPE for healthcare, the challenges that are being faced, and the ways that as a business, you can secure your personal protective equipment (PPE) supply chain.
PPE for Healthcare: A UK Perspective
According to the Covid-19: personal protective equipment (PPE) plan Government policy paper, those most at risk from Covid-19 are professionals working in the health and social care sectors. In response to the pandemic, the government published guidance on appropriate PPE for health and social care workers, in line with World Health Organization (WHO) guidance.
The government also created a central hub on GOV.UK to provide guidance on clinical PPE requirements, developed a parallel supply chain to take pressure of the “normal supply chain,” and created a dedicated system for ordering PPE.
We also held a stockpile specifically for events such as a global pandemic and a no-deal Brexit. The stockpile comprised around 50,000 pallets of medicines and consumables, including PPE and hygiene products. In June, the government announced that since the beginning of the outbreak, 761 million items of PPE had been deployed.
The government predicted that once they had stabilised the distribution of PPE, the supply chain would revert to a more systematic approach based on demand as reported from each trust.
However, throughout this time there have been significant challenges to the distribution of PPE not just in the UK, but on a global scale.
Current best practice with PPE is to store it at a central location, and each department within the trust uses an online portal to order it.
But what if this system doesn’t work? Or the central repository runs out? Or the PPE procured doesn’t actually meet the standards required?
The UK had been preparing for an event such as Covid-19, but still it took us by surprise.
Order batching, where order quantities are distorted, as well as price fluctuations, and poor communication throughout the supply chain has led to a distortion in the supply chain, sometimes known as the “bullwhip effect”.
In order to avoid the effects of this, it is recognised that a single point of control can be most effective. But in the UK, the single point of ordering has proved to be a bottleneck. From testing for Covid-19 to provision of PPE, failings in supply chain management have dominated the news for months.
What went wrong with the Supply Chain Management for PPE?
Supply chain management is about getting the right thing in the right place at the right time. It differs from procurement in that it comes down to timing, which can be critical — no more so than during a global pandemic.
But as we start on the path to recovery, two very hot topics are emerging:
Does the NHS have enough PPE supplies? And can the supply chain cope with the demand for ordering PPE for healthcare?
Back in March, GEP reported on the global struggle to cope with a 100x surge in demand in response to Covid-19. It is not only demand that is surging either — prices are also increasing. In some cases, such as N95 masks, they are costing up to 20 times more than normal.
What is causing disruption to supply chains?
Margeruite Walsh, Vice President for Product Merchandising for Henry Schein, and Chair of the Organization for Safety, Asepsis and Prevention (OSAP) highlighted a number of issues that were disrupting the supply of PPE. Shutdowns in manufacturing as a result of requirements for social distancing, global shortages of raw materials, and issues with product regulatory compliance and government control all played their part in disrupting the supply chain.
When you add to this the above-normal demand, the issues exacerbate massively and hampering the PPE supply chain has put lives and businesses at risk.
What are the solutions to supply chain shortages?
There are a number of ways that supply chain disruptions can be mitigated or smoothed out.
- Increasing manufacturing output and production, and the number of suppliers.
This can help reduce pressure on the normal supply chain. In the UK, businesses were quick to step forward to offer their own PPE stocks to the government and increase production to support the national effort.
- Kingfisher Group (B&Q, Screwfix) donated 240,000 goggles and safety glasses
- Apple donated 215,000 Type II masks
- BP donated 75,000 IIR masks
- Airbus donated over 700,000 IIR masks
Wholesalers including Careshop, Blueleaf, Delivernet, Countrywide Healthcare, Nexon Group, Wightman and Parrish and Gompels were contracted to supply PPE to the social care sector.
- Increasing distribution channels
Optimising distribution channels also alleviates pressure on the supply chain. The government initiated the national supply disruption response (NSDR) system to respond to emergency PPE requests and emergency drops were made to those with urgent PPE requirements.
The Department of Health and Social Care (DHSC), along with its partners NHS England and Improvement, NHS Supply Chain, Clipper logistics, and the armed forces developed a parallel supply chain to support the normal supply chain. This established a dedicated channel for procuring PPE to mobilise critical items to where they were most needed.
A pilot website for ordering PPE was also rolled out, designed to integrate with NHS Supply Chain’s central PPE logistic operations.
- Limiting order sizes
By controlling or limiting order quantities, this can help manage surges in demand. However, rationing is not necessarily an appropriate option for the supply of PPE for healthcare.
- Improved information and communication to measure end-user demand
Many believe that the demand from end-users is more predictable and reliable than the demand experienced by manufacturers. By using end-user demand, and improving communication throughout the supply chain, this can help keep the running level steady.
- Utilising more sophisticated supply chain management methods
As this experience has proved, accurate and intuitive inventory management systems are critical to achieving and maintaining a reliable and continuous supply chain.
Either centralised or decentralised, there must be reliable and comprehensive ordering platforms for end-users to able to request new supplies. These systems must be able to accurately measure the stock they have available in real-time, how much has been used, and by whom, and have the function to set re-order levels to maintain a steady supply.
If ordering platforms are limited in any way, such as to specific contractors or end-users, this limits access to the whole market. As a result, and as we have seen, it is the front line workers and the service users who suffer. These are risks we should not be taking in healthcare.
The future of the PPE Supply Chain and Ordering PPE for Healthcare
As we face second waves of Covid-19, it is clear this pandemic is a problem that is not going to go away anytime soon. It is causing chaos both economically and politically, and businesses must do everything they can to protect their clients and themselves.
Securing supply chains, particularly for PPE, will be critical to how we can survive this crisis. That means having a much clearer understanding of the data: how much PPE is being used, and how much we need. That data, and an accurate system to manage it, is sorely lacking in the current centralised ordering system.
The government guidance on PPE requirements can be found here.
Need to manage your PPE supply chain better?
Enquire and find your StockAssist solution today.
See StockAssist In Action


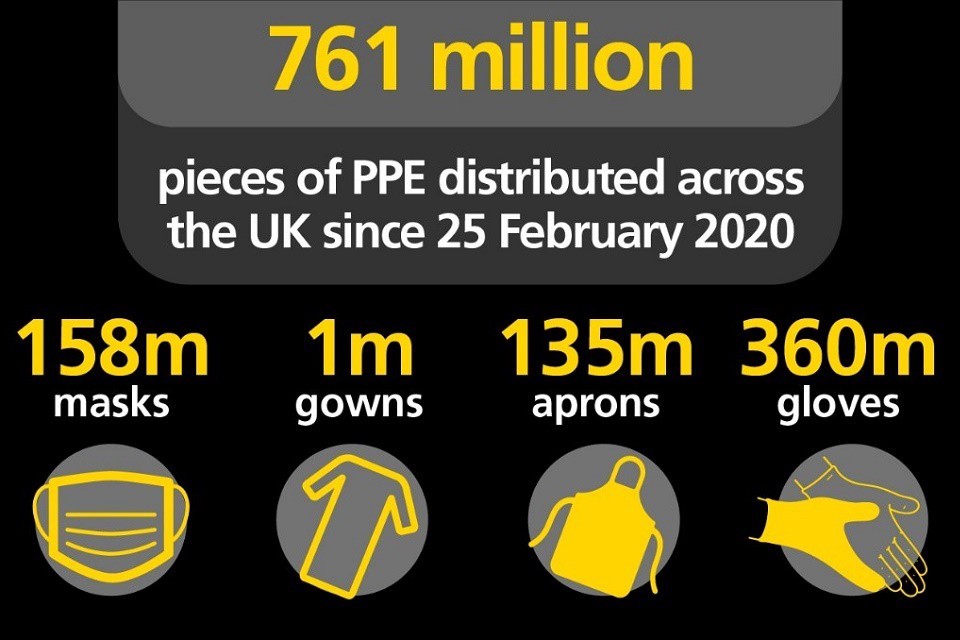 Image credit:
Image credit:  Image credit:
Image credit: 

